Wildlife Disease
What it is
Canine distemper is a highly contagious disease of wild and domestic carnivores. Distemper is caused by a virus that has a broad host range among North American carnivores including the gray fox, raccoons, coyotes, skunks, and weasels. Canine distemper virus is related to rubeola (red measles) but poses no known threat to humans.
Distemper occurs most often in raccoons throughout the Southeastern U.S. and is cyclic in nature, tending to show up approximately every five to seven years. It may appear as sporadic isolated cases or in widespread outbreaks. In wild animals, juveniles are more susceptible to the infection; therefore, the majority of cases are seen in the spring and summer when juvenile populations are at their highest levels. However, distemper outbreaks may occur year-round.
Transmission
A healthy animal may contract canine distemper from direct contact with an infected animal or its bodily secretions and waste. Under most environmental conditions the virus does not survive long outside the body; therefore, transmission requires close interaction between animals to enable direct contact or aerosol exposure.
Infected animals may shed the virus starting approximately five days after infection, for a period of as long as six weeks or until death.
Unvaccinated dogs and cats are susceptible to contracting the disease. Pet owners are reminded to keep their pet vaccinations up to date.
Many of the symptoms displayed by an animal with distemper are very similar to symptoms displayed by a rabid animal (only testing of brain tissue can determine if an animal is rabid). Although distemper poses no threat to humans, anyone bitten or scratched by a raccoon must contact their physician immediately. Exposure to a rabies vector species (raccoons, coyotes, and foxes) may be fatal. Rabies has been documented in East Tennessee and an aggressive oral vaccination program has been initiated.
Clinical Signs
Symptoms of the disease are similar in all susceptible species. The symptoms include distress, coughing, sneezing, diarrhea, discharge from eyes and/or nostrils, eyelids that are crusted over and stuck together, and hardened footpads.
Infected animals may have convulsions, tremors, and chewing fits. These animals may lose their fear of humans, become aggressive, appear blind, stumble, and fall. Infected animals may exhibit stupor, paralysis, coma, and convulsions. An infected animal that is typically nocturnal may be observed in the daylight wandering aimlessly.
Diagnosis
Definitive diagnosis is based on laboratory analysis of affected tissues by fluorescent antibody techniques.
Canine distemper runs its course rapidly. Distemper is often fatal and death is usually attributed to a secondary infection such as pneumonia. Not all raccoons get the disease and many survive the outbreaks.
No specific drug is available that will kill the virus in infected animals. An animal that is symptomatic can not be treated; therefore, infected animals should not be handled by the public.
Other diseases which may mimic distemper include rabies, tularemia, histoplasmosis (raccoons), and poisonings. Raccoon rabies was first documented in East Tennessee in 1993,
Significance
In Tennessee, die-offs of raccoons due to canine distemper occur regularly. Outbreaks of canine distemper may have a significant impact on local or regional populations of raccoons, gray foxes, and skunks in parts of the United States. The transmission of canine distemper is likely density-dependent; the disease poses a threat mainly to concentrated populations of previously unexposed susceptible species.
Canine distemper is of no public health significance to humans.
Dealing With Distemper
- Keep pets and children away from sick raccoons. As the distemper progresses, the animal may appear calm but may become aggressive if approached.
- Feed pets indoors.
- Those who feed their pets outdoors should take special care to remove any leftover food. It can attract infected animals not completely debilitated by the disease.
- Pet owners must get their pets vaccinated.
- Make sure garbage cans are secure and can not be knocked over or their lids removed.
- If you have a compost pile with food scraps, make sure the pile is securely covered in bins that raccoons can not access.
- Sick raccoons may pass through your yard and move on. If a raccoon dies in your yard, bury it deep enough to discourage pets from digging it up, or double bag and dispose of the animal in the trash. Do not touch the animal, and wear rubber gloves when disposing of the animal.
- Never attempt to capture or aid any sick wildlife. Once symptomatic, no treatment is available, and the disease must run its course.
- PLEASE DO NOT FEED THE RACCOONS!! Feeding wild animals may lead to large concentrations of animals around food; therefore increasing the spread of the disease.
What it is
Rabies, also known as “hydrophobia” is a term that frightens many people. Rabies is a fatal disease that affects all mammals including human beings. It is caused by a virus that attacks the central nervous system causing inflammation of the brain.
The virus lives in the saliva of infected animals. The disease is most often transmitted through the bite of a rabid animal. Inhalation of rabies virus has been known to occur, but only in very special circumstances (such as inhalation in confined areas).
Tennessee law requires that all dogs and cats be vaccinated against rabies and that their shots be kept up-to-date. Although cases of rabies in cats in Tennessee are uncommon, there are twice as many rabid cats as dogs in the U.S. To further protect your pets, keep them confined to a controlled area to limit their exposure to wild animals.
The incubation period, the time between exposure to the disease and the onset of symptoms, varies from a few days to several months. The rabid animal may appear healthy while incubating the rabies virus for several months before contracting clinical symptoms and spreading the virus.
Once symptoms begin, there is no treatment for rabies, and is almost always fatal. An animal that has contracted rabies will have flu-like symptoms, severe headaches, and fever. As the disease progresses the animal becomes confused and hallucinates, the brain does not function properly. Many times the animal's jaw will drop, which causes them to drool or foam at the mouth. Foxes and raccoons may be out during the daylight, they will not behave normally.
There are two forms of rabies illness displayed in animals. One form is called furious form rabies, animals with this type of rabies may exhibit early symptoms such as restlessness, agitation, and increased aggressiveness. This is followed by depression, paralysis, and eventually death. The other form of rabies is called dumb form rabies. These animals are lethargic, depressed, partially paralyzed, and may appear unusually tame, they will eventually die. You cannot diagnose an animal with rabies by simply observing the animal and there is no test performed on a live animal that can detect the presence of the rabies virus. In order to test for the presence of rabies brain tissue must be sampled.
The disease can be effectively prevented in humans and many domestic animal species, but abundant and widely distributed reservoirs among wild mammals complicate rabies control. There are many different variants of the rabies virus (skunk-strain, fox-strain, raccoon-strain, bat-strain, etc. Each strain may infect any species of mammal. It is extremely important for people to stay away from wild animals such as bats, foxes, raccoons, and skunks. It is also very important to make sure that all pets are vaccinated.
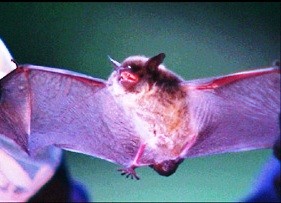
Bat Variant
Most of the recent human rabies cases in the United States have been caused by bats. Since the late 70s, 75% of human rabies cases in the United States have been caused by the bat variant of rabies. Bats have very small teeth, therefore, a bite from a bat may not be detected.
Raccoon Variant
Raccoon rabies is a variant of the virus carried mainly by raccoons. It is spread to other wildlife species, domestic animals, pets, and humans through the saliva of an infected animal in the same way as other variants of rabies. The only difference is that it is spread primarily by raccoons. Raccoons and skunks may incubate rabies for long periods (many months) without becoming ill. They may shed the virus in saliva two weeks prior to showing symptoms.
Raccoon rabies was virtually unknown prior to the 1950s. Florida experienced the first case of raccoon rabies. The disease then spread slowly during the next three decades into Georgia, Alabama, and South Carolina. In 1978 Virginia experienced an outbreak of raccoon variant rabies due to the translocation of raccoons from Georgia and Florida. The first cases appeared in West Virginia and Virginia in the late 1970s. Since then, raccoon rabies in the area expanded to form the most intensive rabies outbreak in the U.S.
The strain now occurs in all the eastern coastal states, as well as Alabama, Pennsylvania, Vermont, West Virginia, Ohio, Maine, and even southern Ontario.
Raccoon rabies was first documented in Tennessee in June 2003. Four positive cases were discovered in raccoons in Carter County and one positive case was found in a feral cat in Johnson County. A second occurrence of raccoon variant rabies was discovered in January 2004. Seven raccoons tested positive for raccoon variant rabies in Hamilton County.
USDA - WS Oral Rabies Vaccine Program
The United States Department of Agriculture and Wildlife Services will be continuing the oral rabies vaccination program which was launched in 2002. Wildlife Services will be distributing oral rabies vaccine (ORV) baits in 16 states in an effort to prevent the westward spread of raccoon rabies in the eastern US. Tennessee will again be participating in the program and plans include counties along the southeastern and eastern borders of the state (portions of Bradley, Carter, Cocke, Greene, Hamilton, Johnson, Marion, McMinn, Monroe, Polk, Sullivan, Unicoi, and Washington Counties).
Sachet baits containing the ORV are coated with an oily, fish-scented substance to attract raccoons and other rabies vector species like skunks, foxes, and coyotes. Each bait is marked with a toll-free number (1-877-722-6725) for people to call for assistance or information if they find or come in contact with the bait. The ORV baits will be distributed by aircraft or car beginning on or about October 4, 2024.
If you find ORV baits, USDA- WS recommends that you leave them alone, unless they are where children or pets play. Please follow these practices to safely move ORV baits:
- Wear gloves when picking up the baits,
- Toss intact baits into a wooded area or other raccoon habitats,
- Bag and place damaged baits in the trash,
- Practice proper hygiene by washing with soap and water any skin or wounds that may have come into contact with the ORV baits, especially if the bait was damaged.
More information about the program can be found on the USDA web pages below.
USDA APHIS | National Rabies Management Program
USDA APHIS | Field Evaluation Continues in Oral Rabies Vaccine for Raccoons, Other Wildlife
In order to efficiently protect the public and monitor the spread of rabies in wild populations, the translocation of all rabies vector species inside the oral vaccination baiting/surveillance zone has been terminated. In Tennessee and elsewhere in the U.S., the number of rabies cases in domestic animals has declined dramatically due to mandatory vaccination laws for dogs and cats. However, rabies among wildlife (especially skunks, bats, and raccoons) has become more prevalent. The higher the incidence of rabies in wildlife, the greater the risk to domestic animals that act as a buffer zone between wildlife and humans.
The Tennessee Wildlife Resources Agency is currently precluded by state law from undertaking any direct rabies control. The Tennessee Department of Health is responsible for the investigation of any potential human rabies exposure.
Rabies Prevention Tips
- Respect and observe wild animals from a distance
- Do not feed wild animals
- Do not approach or handle wild animals
- Secure food and garbage, and do not allow wild animals access to them
- Place trash out for pickup on the same day it will be picked up
- Seal openings in attics, basements, porches, sheds, and barns
- Cap chimneys with screens
- Vaccinate all pets
Avian influenza (Bird Flu or Highly Pathogenic Avian Influenza- “HPAI” is a natural disease among many waterfowl, shorebird, and raptor species.
This flu has little direct effect on waterfowl but occasionally transforms into a strain that can affect poultry and quickly cause mortality. Strains of lethal HPAI have affected poultry facilities in the Pacific Northwest and Upper Midwest. HPAI is not presently known to infect humans.
It is important to consider some precautions that may help reduce the possibility of spreading strains of this disease to poultry in Tennessee.
Specifically, we encourage waterfowl hunters who may raise poultry, work on poultry farms, or visit poultry farms to change all outer layers of their hunting clothing, including boots, before entering any premise that has poultry. The easy way to do this is to wear outer hunting garments that can be taken off before entering poultry facilities, bagging them bag them in black plastic trash bags, and putting them directly into the laundry.
Wear rubber boots that can be treated with bleach before and after entering poultry facilities. Boots can be dipped in a bucket or other container containing a 10% bleach solution and then bagged. It is best to treat boots and remove outer garments before entering your vehicle so that the virus will not be transferred to seats and floors and contaminate other clothing items at a later time.
We believe that a little extra precaution will assist with preventing the spread of any strain of flu that occurs in wild birds to poultry facilities.
Additional resources:
What is Rabbit Hemorrhagic Disease?
Rabbit hemorrhagic disease (RHD) is an emerging wildlife disease caused by rabbit hemorrhagic disease virus type 2 (RHDV2). The disease is highly infectious and has a high mortality rate. RHDV2 affects lagomorphs, members of the Order Lagomorpha, which includes domestic and wild rabbits, pikas, and hares. Susceptible native Tennessee wildlife species include the Eastern Cottontail, Appalachian Cottontail, and Swamp Rabbit. Currently, RHDV2 has not been documented to affect humans or any other animal species.
RHDV2 has an incubation period of 3-9 days. It attacks the liver cells and causes hepatitis. Wild rabbits infected with RHDV2 are often found dead with bleeding from the nose and mouth. RHD usually results in death within 4-6 days after exposure and often the only sign of the disease is sudden death. Infected animals which live longer or survive the disease may develop respiratory and neurological symptoms, fever, lethargy, and a decreased appetite and can shed the virus for 30 days.
Caution should be taken when handling rabbits that are suspected to have died from RHD as the clinical signs are the same as tularemia (rabbit fever) which can cause disease in people.
Distribution of RHDV2 Outbreak in the US
RHDV2 was first detected in France in 2010 and was found in North America in a wild rabbit in April 2020. It has since been confirmed in wild lagomorphs and/or domestic rabbits in 17 states. A stable-endemic area of RHDV2 exists in Texas and much of the contiguous western United States. In these states, RHDV2 has been documented in domestic rabbits and wild lagomorphs. Outside of the endemic area, domestic cases have been confirmed in Florida, Georgia, Kentucky, Mississippi, Minnesota, and South Dakota. In January of 2022, RHDV2 was detected in two domestic rabbits in east Tennessee. Although RHDV2 has not yet been found in Tennessee’s wild rabbit populations, this is a concern due to the high infection and mortality rates of the virus.
The USDA conducted genetic sequencing of RHDV2 in domestic rabbits in Florida and Georgia and found the viruses may be connected to the western outbreak rather than from new introductions. This suggests a risk of movement of RHDV2 across the landscape.
To view an interactive map of the current outbreak, Visit the United States Department of Agriculture (USDA) website at to view an interactive map of the current outbreak.
How is RHDV2 Spread?
RHDV2 can be found in feces, urine, and respiratory secretions of infected animals and can be passed to uninfected animals either through direct or indirect contact. The virus can survive in the environment for 3-4 months and can be passed indirectly to uninfected animals through contaminated food, bedding, water, and carcasses. Scavengers, like birds or insects, may act as vectors to transmit the virus to new areas. People may also unintentionally spread the virus on our hands, clothes, and shoes or by moving live or dead rabbits.
Preventative Measures
The following preventative measures are recommended for hunters and rabbit owners to limit exposure and spread of RHDV2:
Hunters & Falconers
- Avoid harvesting rabbits that appear sick.
- When processing rabbits wear disposable gloves.
- Disinfect equipment and wash hands.
- Prepare meat to an internal temperature of at least 165°F.
- Bury rabbit remains to discourage scavenging.
Rabbit Owners
- Keep rabbits indoors or keep rabbit enclosures raised and off the ground.
- Wash hands, clothes, and shoes before and after contact with domestic rabbits.
- Do not handle dead or wild rabbits.
- Quarantine new domestic rabbits for at least 30 days from other animals.
- Notify the State Veterinarian’s office if you experience sudden deaths or high mortality in your rabbitry at (615) 837-5120 or animal.health@tn.gov.
RHDV2 Vaccine
A vaccine for RHDV2 to be used in domestic rabbits is now available in over 40 states including Tennessee. The vaccine was produced by Medgene Labs and was granted Emergency Use Authorization by the USDA Center for Veterinary Biologics in October of 2021. The vaccine has been effective in preventing the severe and fatal disease from RHDV2 infection in domestic rabbits but is meant as a supplement to the above preventative measures.
Additional Resources
TWRA Printable RHDV2 Fact Sheet
Tennessee Department of Agriculture RHDV2 Information Page


