Mental Well-Being
Across Tennessee, the United States, and the world, people have been facing increasing challenges with their mental health and well-being. Encompassing our emotional and psychological wellness, mental health is critical in how we cope with stressful situations, connect to others, make healthy choices, and function on a daily basis. Beyond surviving, we want to thrive too. Mental well-being involves one’s ability to find meaning in what they do, strive for continual self-growth, and feel a sense of self-worth.
Everybody has mental health, just like we all have physical health. Even if you don’t experience a specific mental health condition, you may still deal with issues that negatively affect your mental health and well-being. It is important to care for our mental well-being even outside of times of crisis and work to create communities where others can thrive as well.
Some factors that can impact our mental health include:
- Biological factors
- Life experiences (trauma, abuse, etc.)
- Family history of mental health problems
- Adverse Childhood Experiences (ACEs) such as a history of abuse or having a parent with mental illness
- Experiences related to other ongoing chronic medical conditions (cancer, diabetes, etc.)
- Adverse Community Experiences such as community violence or concentrated poverty
Mental illness refers to a wide range of mental health conditions or disorders that can affect an individual's mood, behavior, and thinking. Examples of these conditions include depression, anxiety disorders, schizophrenia, eating disorders, and addictive behaviors. In the United States, mental illnesses are among the most common health conditions.
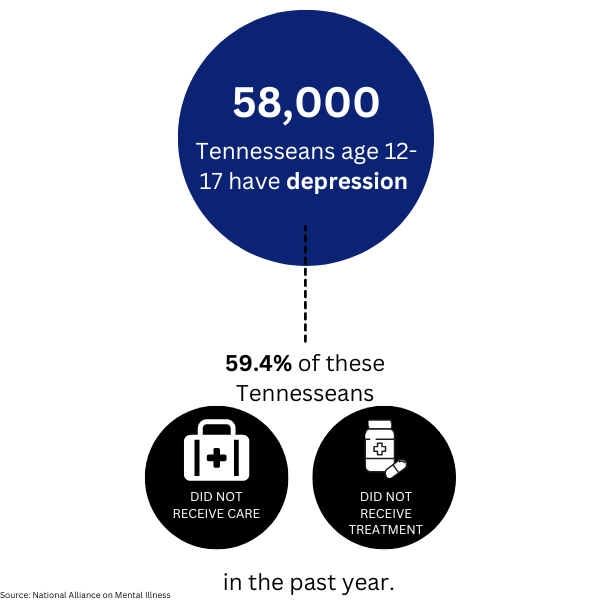
In Tennessee,
- 18% of adults experienced frequent mental distress in 2021
- Adult suicide mortality rate was 22.00 per 100,000 in 2021
- 1 in 4 children has a mental, emotional, developmental, or behavior disorder
- 71% of youth with major depressive disorder did not receive health services
- 144 deaths by suicide occurred among those under 24 in 2020
When addressing mental health and well-being in our communities, we have two priorities — making sure those experiencing poor mental health are able to access the resources they need to get better, and creating the community-wide conditions that prevent this distress and ensure well-being for all.
Our state of mental well-being, and how we are able to treat issues when they arise, is often directly impacted by the community around us. Community conditions like the environments we live in, the jobs we can find, and the healthcare services we can access and afford all influence our ability to cope with daily stressors. They can even have an impact on the intensity and frequency of psychotic episodes we experience. By improving community conditions along with having high-quality mental health services, our society can reduce the likelihood, frequency, and intensity of mental health challenges in our communities while also improving our physical health outcomes.
Mental well-being is important for a variety of reasons and can help us with:
- Coping with the stresses of life
- Maintaining healthy relationships
- Making meaningful contributions to our community
- Work/school productivity
- Feeling a sense of self-worth
Mental health can also impact your physical health. Mental disorders can increase your risk of serious health conditions such as strokes, type 2 diabetes, heart disease, and more. Individuals who struggle with their mental health may turn to substance use, which can in turn worsen mental health symptoms alongside physical risks.
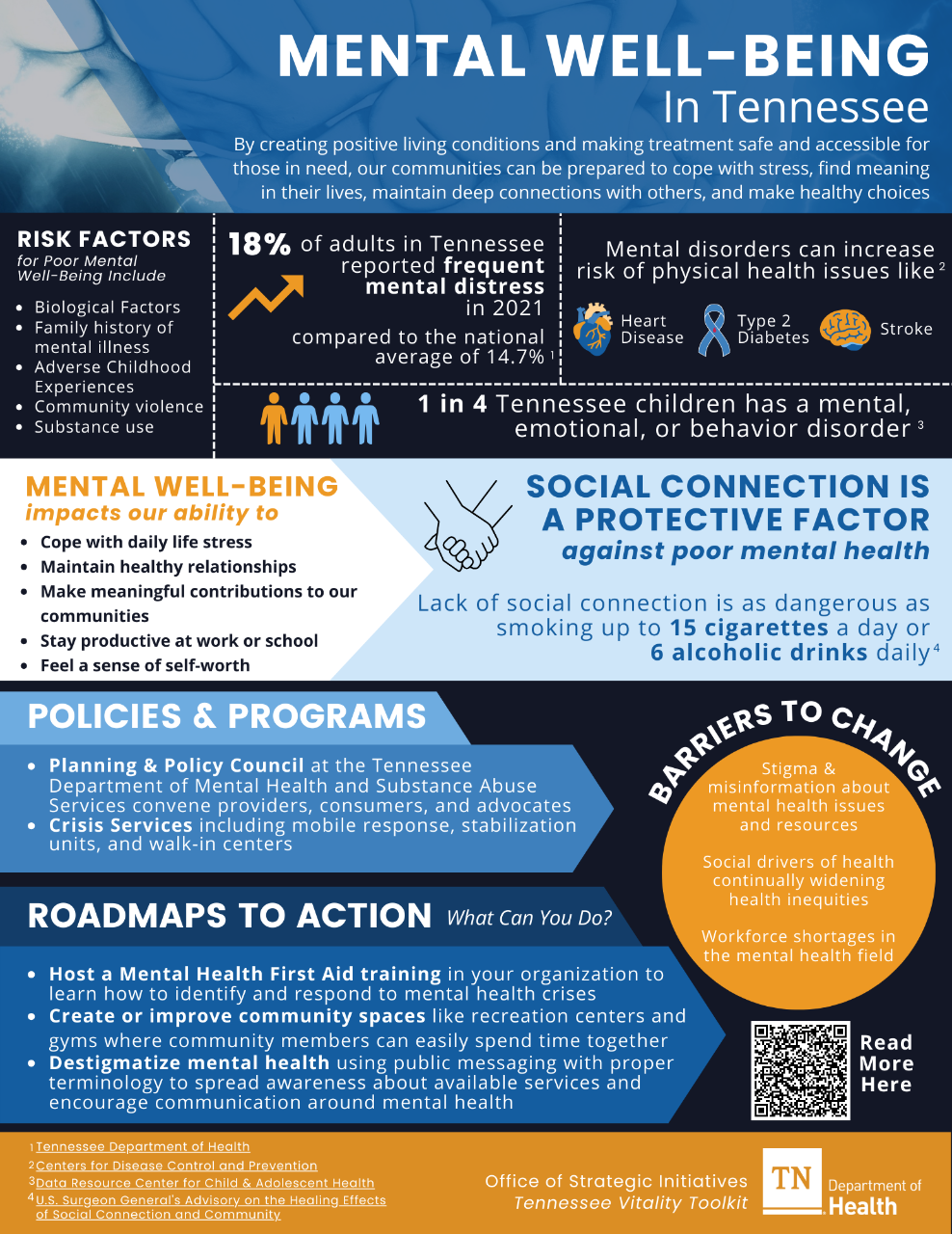
Luckily, we can strengthen our mental well-being and that of those around us through is the relationships, connections, and interactions we have with family, friends, colleagues, neighbors, and our community. Social connections are essential to our mental well-being. Various studies have shown that those who are more socially connected live longer than those who experience social deficits such as isolation, loneliness, and poor-quality relationships regardless of the cause of death. In fact, the lack of social connections is as dangerous as smoking up to 15 cigarettes a day or drinking 6 alcoholic drinks daily, according to the Office of the U.S. Surgeon General.
Communities have the power to come together and create the conditions that make good mental health and well-being possible. Instead of leaving individuals to face these challenges on their own, we can use community-wide strategies to create positive living conditions and, when mental health crises arise, make treatment safe and accessible.
Everyone has the potential to face mental health challenges. However, because community and social conditions impact our mental health so directly, certain groups face particular risks for mental distress.
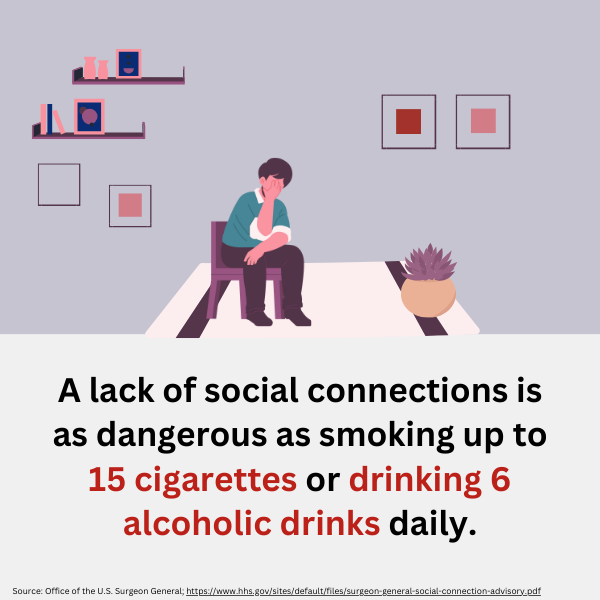
Adults
In Tennessee, 937,000 adults have a mental condition. For reference, this is about 5x the population of Knoxville. In 2021, 1,220 lives were lost to suicide in Tennessee. In the United States, 1 in 5 adults experience mental illness each year.
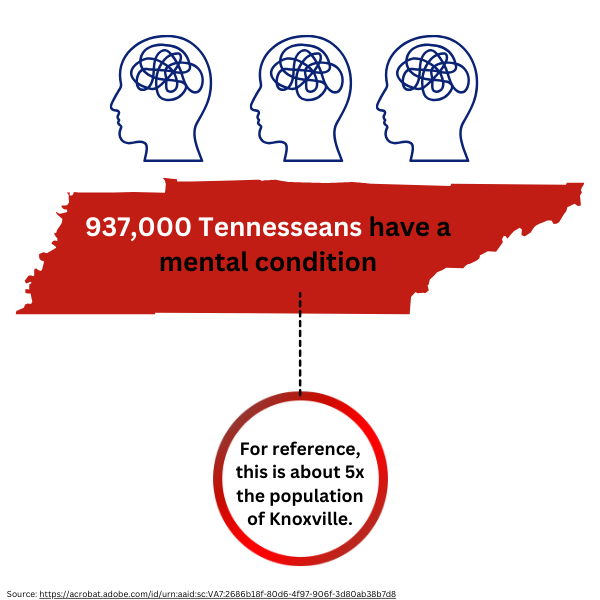
Youth
58,000 Tennesseans ages 12 to 17 have depression, and 59.4% of Tennesseans in that age group who have depression did not receive any sort of care or treatment in the last year, according to the National Alliance on Mental Illness. High school students with depression are twice as likely to drop out compared to their peers. In the United States, 1 in 6 youth between the ages 6 to 17 experience a mental health disorder each year.
Incarcerated Individuals
In the United States, 7 in 10 youth in the juvenile system have a mental health condition. 1 in 4 people with a serious mental illness have been arrested by the police at some point in their lifetime. This leads to over 2 million jail bookings of people with serious mental illness each year. About 2 in 5 adults in the United States who are in jail or prison have a history of mental illness.
Uninsured/Underinsured Individuals
Over 11% of Tennesseans in 2021 were uninsured. Even for those who do have insurance, Tennesseans are over 6x more likely to be forced out-of-network for mental health care than for primary health care. High out-of-pocket costs leave individuals unable to afford necessary care. Tennessee, like many other parts of the United States, is facing a mental health professional shortage. Over 3,224,000 individuals in Tennessee live in a community that does not have enough mental health professionals.
Unhoused Individuals
In 2021, there were about 7,256 unhoused individuals in Tennessee.1 in 6 people experiencing homelessness live with a serious mental illness.
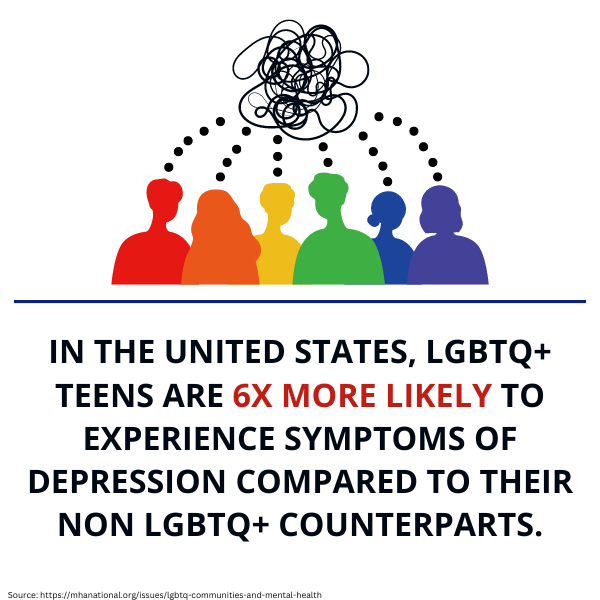
LGBTQ+ Individuals
In the United States, LGBTQ+ teens are 6x more likely to experience symptoms of depression compared to their non-LGBTQ+ counterparts. Gay, lesbian, and bisexual youth are more than 2x as likely to feel suicidal and over 4x as likely to attempt suicide when compared to heterosexual youth. 48% of transgender adults reported that they have considered suicide in the last year compared to 4% of the overall U.S. population, according to the 2015 U.S. Transgender Survey.
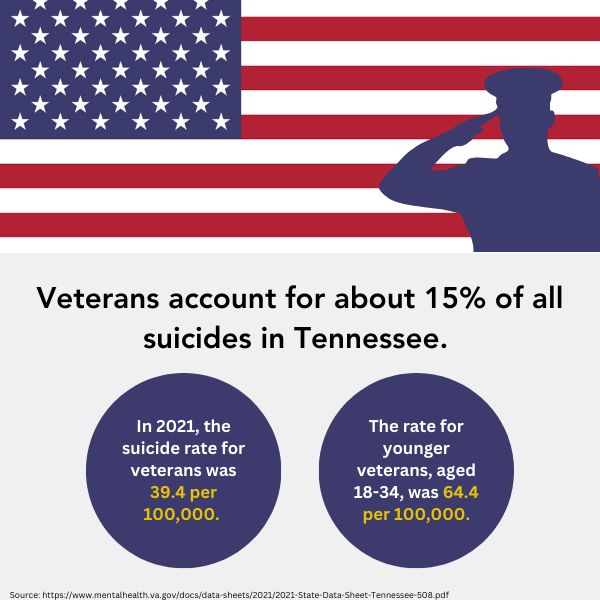
Veterans
In Tennessee, the suicide rate of veterans was 39.4 per 100,000 in 2021. This rate was even higher for younger veterans, with the suicide rate for those aged 18-34 at over 64 per 100,000. Veterans accounted for about 15% of all suicides in Tennessee.
Activities and Programs: Evidence-informed, actionable, short-term steps that collaborative groups can take to address priority areas.
Policy and Systems Change: Systems change refers to how organizations or programs — such as school systems or health systems — are connected and work together to improve conditions to make change that lasts. This section contains evidence-informed, actionable, long-term steps that collaborative groups can take to address priority areas.
- Create community programs where neighbors can connect and students can establish social skills, and generate opportunities for high-risk populations to create a sense of community and build relationships.
- Host community events that bring community members together to socialize and build relationships. This can include game nights, neighborhood BBQs, movie nights, and farmers markets with local businesses as partners.
- Create or improve community spaces like recreation centers or gyms, providing members of your communities with safe places, both indoor and outdoor, where they can gather, hangout, and hold events.
- Start reducing the stigma around mental health by talking openly about mental health, educating your community, and being conscious about the language you use surrounding mental health.
- Host a training on Mental Health First Aid to teach community members how to identify and respond to mental health crises. To inquire about hosting a training through the Department of Health, email MHFA.training@tn.gov.
- Increase access to safe green spaces like parks and gardens. Spending more time outdoors in nature has been shown to have positive impacts on reducing our stress, improving our moods, and decreasing our risk for developing a mental health condition. Check out the Office of Primary Prevention’s list of funding opportunities related to that topic.
- Create intergenerational programs that increase connections and support the development and maintenance of relationships between youth and older adults. Creating programs that bring youth and older adults together and foster relationships between them.
- Support policy initiatives that address root causes of desired mental health goals. Conduct a root cause analysis to explore factors that contribute to particular mental health challenges for your community. Conducting a root cause analysis will allow you to identify and tackle the underlying causes surrounding mental health and help you to strengthen your community.
- Get involved with a Regional Policy and Planning Council. These groups are made up of mental health and substance abuse service providers, consumers, family members, advocates and other stakeholders that advise the Tennessee Department of Mental Health and Substance Abuse Services about the service system, policy development, legislation, budget requests, system evaluation and monitoring.
- Influence policy and legislation by exploring opportunities to incorporate community prevention strategies into already-existing mental health policies and regulations.
- Encourage community institutions such as healthcare, education, housing and development, and business, to include community mental health as a priority in activities such as hiring, purchasing, and workplace policy development.
- Engage community leaders in collaborations with multiple sectors (including health, education, criminal justice, law enforcement, business, housing and more) in order to explore strategies that advance community well-being.
- Bring together mental and behavior health practitioners to discuss implications and opportunities to advance community prevention that can complement treatment and early intervention strategies.
Trousdale County Mental Health Services Center
For the past few years, the Trousdale County Health Council has been collaborating with the Mayor's office to coordinate the Mayor's Task Force for Mental Health and Substance Abuse. In 2021, Trousdale County experienced 6 suicides - an alarming rate for a small community of 11,000 people. In response, the task force was formed to create a coordinated effort to bring mental health resources to the county. The task force is a multisector group with community involvement from faith-based organizations, behavioral health organizations such as Centerstone and Volunteer Behavioral Health, the sheriff and district attorney, and more. At the time the task force was being formed, there were virtually no mental health resources available in the entire county.
One of the key goals of the task force was to procure a building to offer mental health services where providers could have a home base. Through the partnership with the mayor's office and the county, the task force received funding for $80,000. The task force found a space where services could be offered in a building that also houses a pharmacy and a medical provider, helping to eliminate small town stigma from keeping people from services. They partnered with multiple behavioral health providers to share the space so that individuals could seek treatment from any of the available providers - including Volunteer Behavioral Health, Centerstone, HOPE Clinic, and Senior Solutions. The new mental health services center celebrated their kickoff in June 2023, and have already enrolled various community members to receive services. The original funding will support the project for the initial pilot period of 2 years, with the hope that the mental health services center can become embedded into the Trousdale community for years to come. This successful collaboration between the Health Council, the Mayor's office, and multiple community partners is already making a difference in access to mental health providers in Trousdale County.
For more information about this story, contact Kathy Atwood at kathyatwood@tcschools.org.
Tennessee Department of Mental Health & Substance Abuse Services
- TN Statewide Crisis Hotline is free and available 24 hours a day, 365 days a year. It is a resource for anyone who is experiencing a mental health crisis. All calls are routed to a trained crisis counselor in your area who will provide you with support, guidance, and work to connect you with appropriate community support.
- Map of Statewide Crisis Services provides a map of mobile crisis teams, crisis stabilization and walk in clinics, regional mental health institutes, respite services, and medically monitored withdraw management.
- Mobile Crisis Services is a 24/7 response team for those who are experiencing a mental health emergency.
- Crisis Services for Children and Youth are provided by Youth villages, Mental Health Cooperative, Frontier Health, and the McNabb Center across Tennessee. There are emergency counselors (triage specialists) that handle calls 24/7 through their regional hotline and determine an appropriate response.
- Crisis Walk-in Centers offer face-to-face, 24/7/365 evaluation for those who are experiencing a mental health emergency. To find a walk-in center closest to you, call 855-CRISIS-1 (855-274-7471)
- Crisis Stabilization Units (CSU) offer 24/7/365 intensive, short-term stabilization for someone who is experiencing a mental health emergency and is willing to receive services. The average CSU stay length is 3 days and the service is free of charge.
- Suicide Prevention Programs offer a variety of services that provide prevention and postvention for those who are experiencing suicidal thoughts or a post suicidal crisis including family support to those who have completed suicide.
- Crisis Intervention Teams (CIT) improve the outcomes for people living with mental health challenges who encounter law enforcement. CIT training is a specialized 40-hour program for law enforcement officers and is in conjunction with robust community partnerships. The goal is to improve outcomes of encounters with people living with behavioral health challenges.
- “Be the One” Suicide Prevention Campaign is a training that equips staff members with the tools and resources necessary to recognize when someone they know may be thinking about suicide. It teaches how to ask the questions directly and offers tips on how to develop good listening skills which are a key component of suicide prevention. The training also provides individuals with the tools necessary to instill hope when someone you know seems have lost all hope.
- Behavioral Health Safety Net (BHSN) services are available for anyone who is 3 years of age or older, has a qualifying mental health diagnosis, and does not have behavioral health insurance. Services provided by this program include assessment, evaluation, diagnostic, therapeutic intervention, case management, transportation, peer support services, psychosocial rehabilitation services, psychiatric medication management, labs related to medication management and pharmacy assistance, and coordination.
- Regional Mental Health Institutes (RMHI) are operated by The Tennessee Department of Mental Health and Substance Abuse Services and are located in Bolivar, Chattanooga, Memphis, and Nashville. All four RMHIs are accredited by The Joint Commision and have deemed status with the Centers for Medicare and Medicaid Services. The program also contracts with three privately-run psychiatric hospitals in East Tennessee for involuntary admissions to inpatient psychiatric treatment.
- On Track TN: First Episode Psychosis Initiative is designed to provide early intervention for youth and young adults between the ages of 15 to 30 who have experienced first-episode psychosis. This comprehensive intervention model involves a team of mental health professionals and support services, focusing on helping people work toward recovery and meeting personal goals.
TN Voices
- TN Voices promote the use of a coordinated system of care in Tennessee that includes family support and community engagement as key components. TNV works collaboratively to ensure that the services being provided to children and families in Tennessee are family driven, community based, and culturally and linguistically competent.
Rural Health Information Hub
- Mental Health in Rural Communities Toolkit compiles evidence-based and promising models and resources to support organizations implementing mental health programs in rural communities with a primary focus on adult mental health.
US Department of Veterans Affairs
- Veterans Crisis Hotline is a 24/7 confidential crisis support for veterans and their loved ones. You do not have to be enrolled in VA benefits or health care to call.
Substance Abuse and Mental Health Services Administration (SAMHSA)
- Community Conversation about Mental Health: Information Brief Toolkit is designed to help individuals and organizations who want to organize community conversations achieve three potential objectives: get others talking about mental health to break down misperceptions and promote recovery and healthy communities; find innovative community-based solutions to mental health needs, with a focus on helping young people; and develop clear steps for communities to address their mental health needs in a way that complements existing local activities.
Centers for Disease Control and Prevention (CDC), About Mental Health
- Adults Who Experience Mental Illness Each Year, 2024
Centers for Disease Control and Prevention Morbidity and Mortality Report, Sexual Identity, Sex of Sexual Contacts, and Health-Related Behaviors Among Students in Grades 9–12 — United States and Selected Sites, 2015
- Gay, Lesbian and Bisexual Youth Statistics on Feeling Suicidal and Likelihood to Attempt Suicide, 2015
Kids Count, State of the Child 2022
- Children with a Mental, Emotional, Developmental or Behavior Disorder, 2022
- Youth with a Major Depressive Disorder Who Did Not Receive Health Services, 2022
- Deaths by Suicide Among Those Under 24, 2022
Mental Health America (MHA), LGBTQ+ Communities and Mental Health
- LGBTQ+ teens in the U.S. who Experience Symptoms of Depression, 2018
National Alliance on Mental Health, Mental Health Conditions
- U.S. Youth Aged 6-17 Who Experience a Mental Health Disorder Each Year, 2021
National Alliance on Mental Illness (NAMI), Mental Health in Tennessee
- Adults in Tennessee with a Mental Condition, 2021
- Tennesseans Ages 12 to 17 Who Have Depression, and Who Did Not Receive Any Sort of Care or Treatment in the Last Year, 2021
- Youth in the U.S. Juvenile System Who Have a Mental Health Condition, 2021
- People with a Serious Mental Illness Who Have Been Arrested by the Police, 2021
- Jail Bookings of People with Serious Mental Illness Each Year, 2021
- Adults in the United States Who Are in Jail or Prison Have a History of Mental Illness, 2021
- Uninsured Tennesseans in 2021, 2021
- Tennesseans with Insurance being Forced out-of-network for Mental Health Care, 2021
- Tennessee Individuals Who Live in a Community Lacking Mental Health Professionals, 2021
- Number of Unhoused Individuals in Tennessee, 2021
- Individuals Experiencing Homelessness Who Live with a Serious Mental Illness, 2021
National Center for Transgender Equality, The Report on the 2015 Transgender Survey
- Transgender Adults who Reported Having Considered Suicide in the Last Year
Revisiting the Link Between Depression Symptoms and High School Dropout: Timing of Exposure Matters, 2018
- High School Students with Depression, 2018
Tennessee Department of Health, Suicide Prevention in Tennessee 2022 Annual Report
- Lives Lost to Suicide in Tennessee, 2021
Tennessee Department of Health, The State of Health in Tennessee
- Adults Experiencing Frequent Mental Distress, 2021
- National Average for Frequent Mental Distress, 2021
- Adult suicide mortality rate in Tennessee, 2021
U.S Department of Veterans Affairs, Tennessee Veterans Suicide Data Sheet 2021
- 2021 Suicide Rate of Veterans in Tennessee, 2021
- Suicide Rate for Veterans Ages 18-34 in Tennessee, 2021
- Veteran Suicides in Tennessee, 2021
U.S. Surgeon General’s Advisory on the Healing Effects of Social Connection and Community, Our Epidemic of Loneliness and Isolation
- Social Connections, 2023