Access to High Quality Healthcare
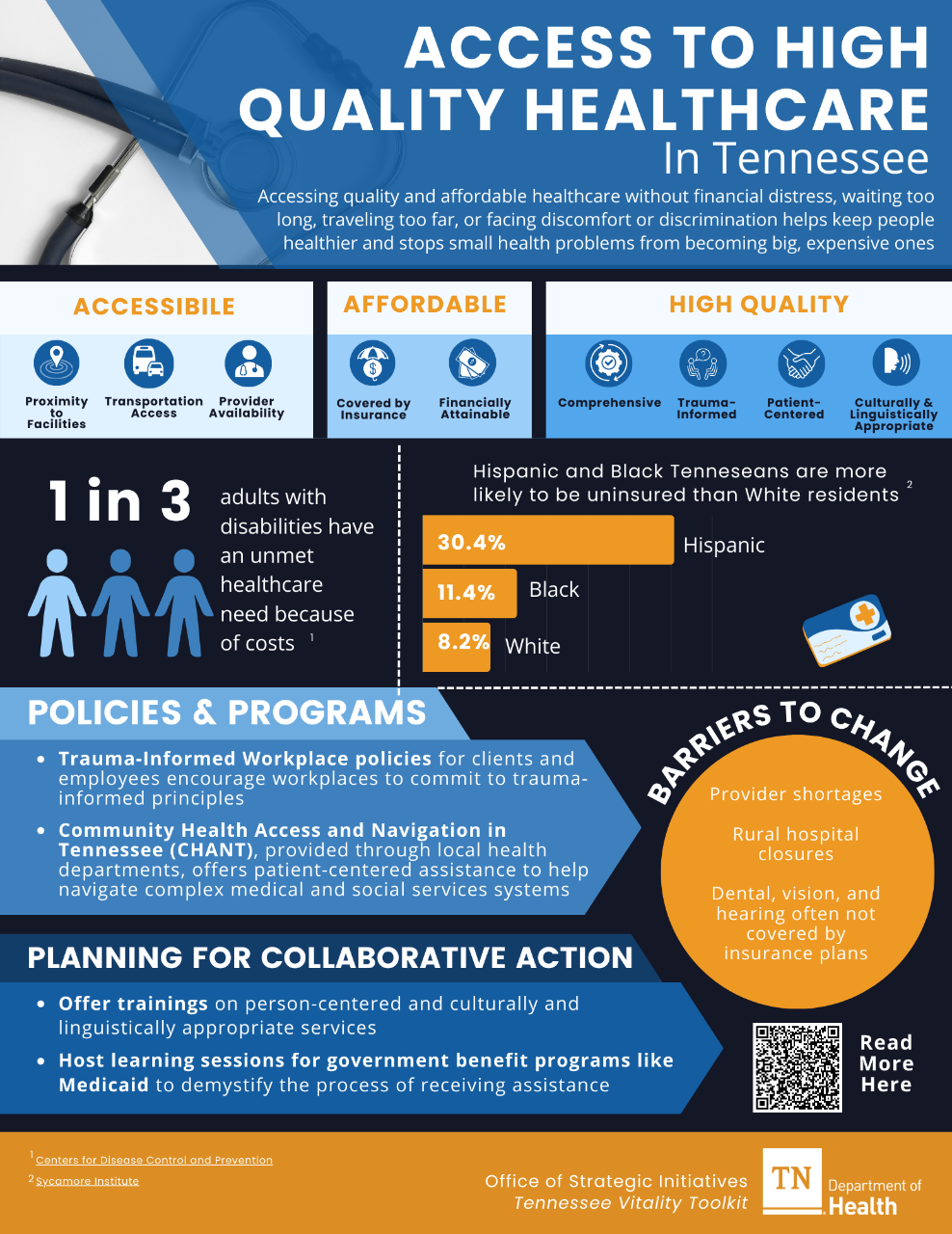
Accessing quality and affordable healthcare means that people can get the medical help they need without financial distress, waiting too long, traveling too far, or facing discomfort or discrimination during their healthcare experience. This helps keep people healthier and stops small health problems from becoming big, expensive ones.
Tennessee currently faces provider shortages in physicians, dentists, and mental health care providers; meaning that a large proportion of our state face barriers to reaching a provider when they need one. Accessible healthcare refers to:
- Proximity: Are healthcare facilities located near where residents live?
- Transportation: Do residents have a way to get to and from appointments? Are clinics located along public transportation routes?
- Provider availability: Are there enough healthcare providers to meet the needs of the community? Are wait times reasonable?
When people can see providers without breaking the bank or going into debt, they are more likely to seek out care when they need it. Affordable healthcare refers to:
- Insurance: Do people have health insurance to cover the cost of medical, dental, and mental health care? Does the clinic accept Medicaid?
- Financially Attainable: Are there resources available to help break down financial barriers to care? Does the clinic offer sliding scale services or a financial assistance policy (FAP)?
When people feel comfortable, heard, and respected in healthcare settings, they are more likely to trust their providers, follow up with treatment, and feel empowered in achieving their health goals. High-Quality healthcare refers to care that is:
- Comprehensive: Can people access an array of services (mental and physical) in one setting?
- Trauma-Informed: Do people feel comfortable, heard, and respected in healthcare settings?
- Patient-Centered: Do providers treat patients as people first, rather than only as a disease or problem to be fixed?
- Culturally and Linguistically Appropriate: Can providers meet diverse language and cultural needs of patients?
Addressing these factors is vital to ensuring everyone can benefit from quality healthcare services.
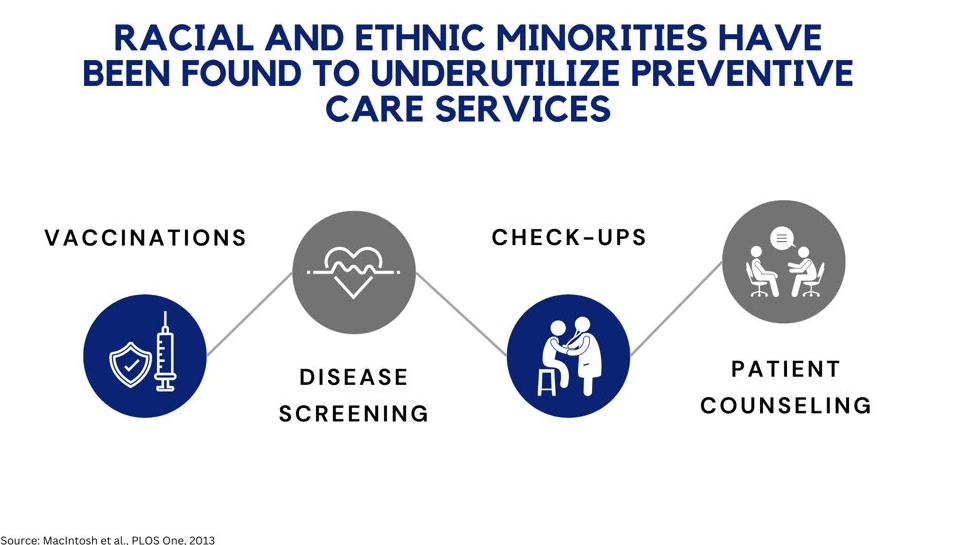
Communities that can access affordable and high-quality healthcare tend to be healthier overall. Patients with a trusted primary care provider are more likely to seek preventative care, such as check-ups, vaccines, and screenings. They are also more likely to contact a doctor more quickly if they have a health concern.
Healthcare organizations can also act to improve communities in ways that support health. For example, hospitals can partner with County Health Councils to align their federally mandated Community Health Needs Assessment (CHNA) with the work of the Community Health Improvement Process, increasing community engagement while addressing the social drivers of health. Strengthening this relationship between the community and the hospital streamlines efforts within a community to improve overall health.
Quality healthcare isn’t just about treating illnesses; it’s also about preventing them in the first place. Quality healthcare supports patients with preventative care, treatment, comprehensive care, and works to improve the social and community needs that impact our health. Together, these efforts stop diseases from spreading, help people live healthier lives, and make changes to communities that support healthy living.
When people are healthier, they can work better and contribute to the growth of the community. Having access to quality and affordable healthcare keeps everyone healthier and makes the whole community stronger over time.
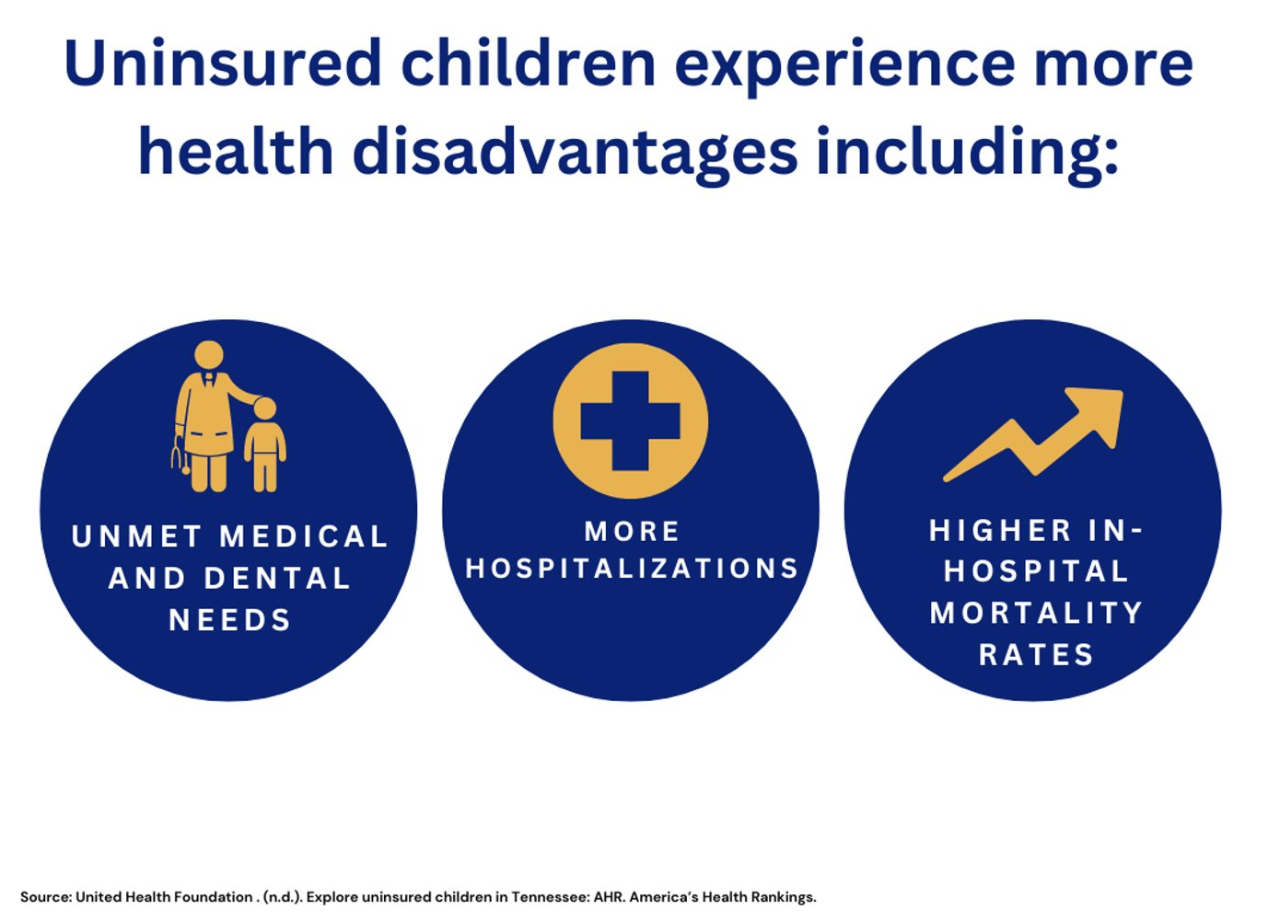
Certain communities face disproportionate barriers to accessing high-quality care, including uninsured Tennesseans, racial and ethnic minorities, Tennesseans living in rural areas, adults with disabilities, people with limited English proficiency, and older adults. These barriers prevent individuals from seeking healthcare, resulting in worse health overall.
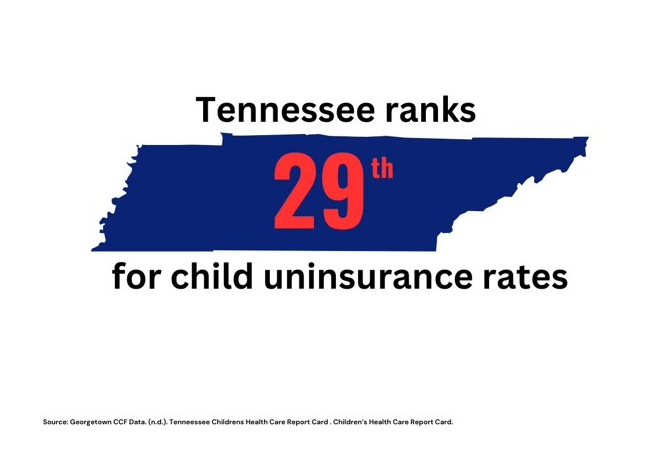
Uninsured Tennesseans
In Tennessee, certain communities face higher uninsurance rates than others. The rate of uninsured children in Tennessee between the ages of 6 to 18 is 5.4% and the rate for children under the age of 6 is 3.8%. This is largely due to health literacy barriers; through the CoverKids program, many children are eligible for insurance - but many families are unaware, leaving children without essential coverage.
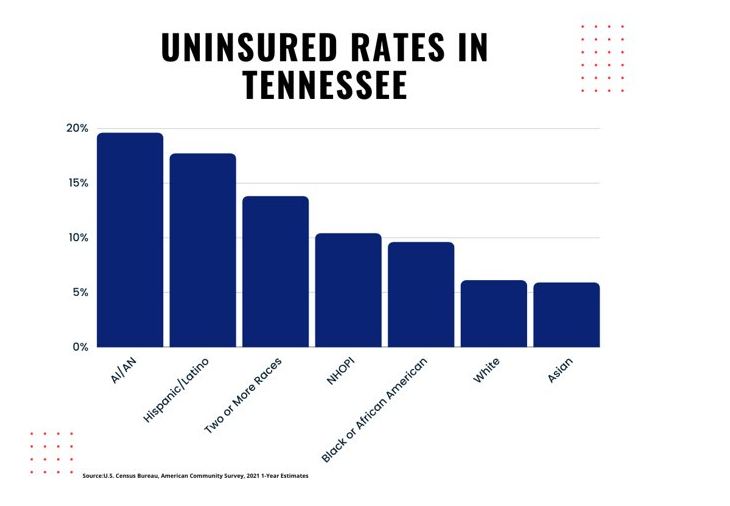
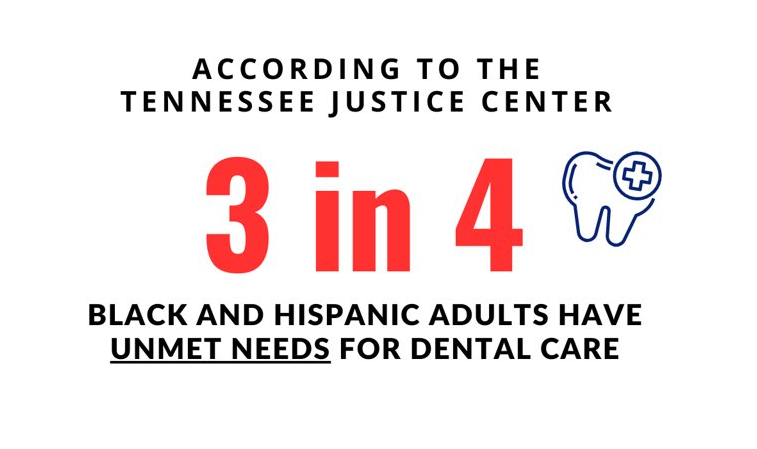
Racial and Ethnic Minorities
Racial and ethnic minorities are more likely to report discrimination in healthcare, resulting in avoiding healthcare altogether. In a recent study by the Pew Research Center, 56% of Black Americans reported at least one substantial negative experience in healthcare, and 49% reported that they believe poor health among Black Americans is caused by poor medical care offered to black patients.
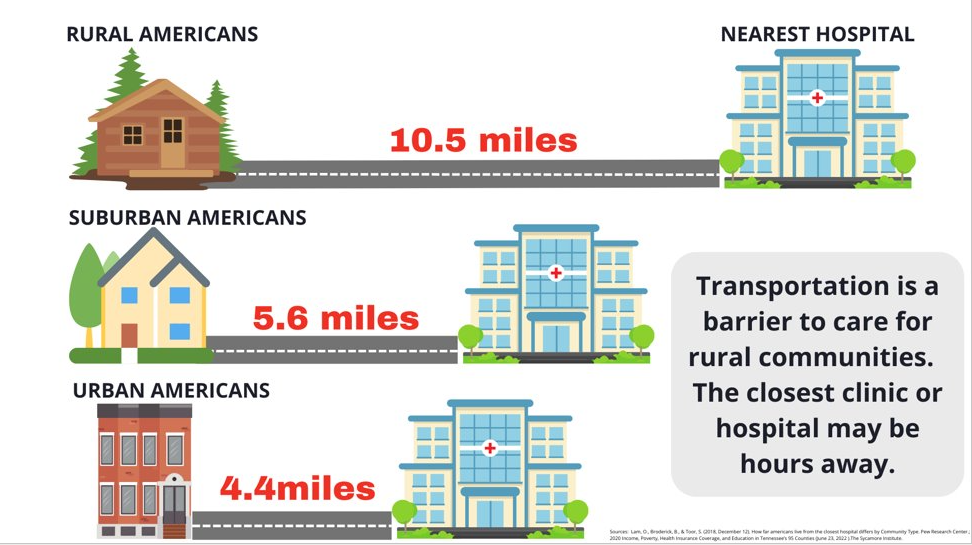
Rural Communities
Rural Tennesseans face significant transportation barriers to access care, limiting their ability to get treatment when they need it or attend preventative visits regularly.
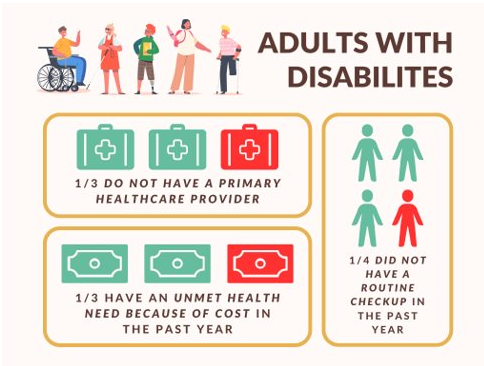
Adults with Disabilities
Adults with disabilities are more likely to face barriers to accessing care, affecting their overall health over time.
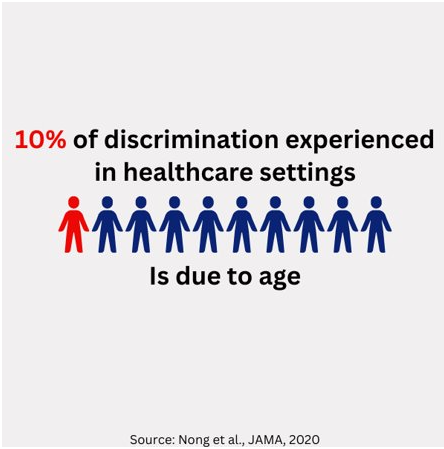
Older Adults
Older adults not only face financial barriers to healthcare, but they also report high levels of discrimination in healthcare. Many older adults are retired and live on fixed incomes. The high costs associated with care put a considerable financial strain on their already fixed incomes.
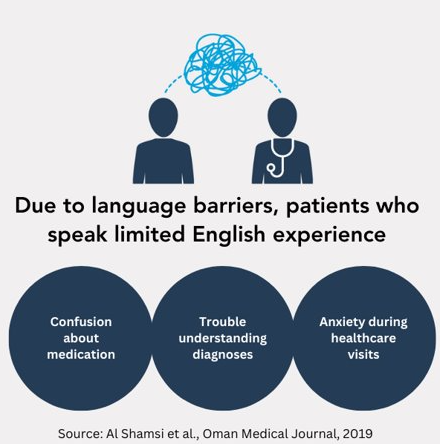
Individuals with Limited English Proficiency
Due to language barriers, patients with limited English language skills report confusion using medication, trouble understanding their diagnosis, and anxiety with healthcare visits in general.
Activities and Programs: Evidence-informed, actionable, short-term steps that collaborative groups can take to address priority areas.
Policy and Systems Change: Systems change refers to how organizations or programs – such as school systems or health systems – are connected and work together to improve conditions to make change that lasts. This section contains evidence-informed, actionable, long-term steps that collaborative groups can take to address priority areas.
- Promote local health department services. CHANT is an integrated model of care coordination that is provided through local health departments. The program provides patient-centered assistance to help navigate the complex systems and care coordination of medical and social service needs, including:
- Dental
- Primary Care
- Immunizations
- Behavioral Health
- Pregnancy/Postpartum
- Social Service Support
- Visit the TDH CHANT page to learn more
- Connect community members to assistance programs such as TennCare (Medicaid) and Coverkids (CHIP). Navigating government resources can be overwhelming. Providing community resources, workshops, and partnering with organizations that help individuals access these programs can help remove barriers and increase access to care.
- Host learning sessions for government benefit programs such as SNAP, WIC, and Medicaid. Lack of information about government programs can be a large barrier that keeps people away from health resources. Hosting an event or providing community resources that demystify this process can increase access for families, supporting increased economic stability.
- Offer trainings in person-centered and culturally and linguistically appropriate services during staff onboarding or professional development. Health Councils can provide trainings for the council, then let representatives go back to their own organizations as spokespeople. This can improve the quality of healthcare services and build trust within communities and their healthcare providers.
- Adopt Trauma-Informed Workplace policies, which encourage workplaces to commit to trauma-informed principles. Trauma-informed workplaces lead to organizations skilled at implementing trauma-informed care, increasing community resilience and cohesion. Health Councils can learn together how to adopt trauma-informed workplace policies in the organizations they represent and can promote trauma-informed policies for their local governments.
- Speak with local healthcare providers about the importance of hiring interpreters, especially if your community has a large population of individuals with limited English proficiency.
- Participate in a Patient/Family Advisory Council. These councils provide opportunities for healthcare organizations to better understand perspectives of patients and families, and build trust between patients, families and providers. Because a patient’s health affects more than just the patient, successful family engagement can support the health and wellbeing of the entire family.
- Support free or sliding scale medical clinics which increase access to healthcare beyond the services available at most health departments. Partnering to promote and expand the reach of these income-based medical clinics can reduce the risk of medical debt and increase access to healthcare for all.
- Support efforts to improve screening in healthcare for factors that may get in the way of seeking treatment, such as transportation, cost, and other social drivers of health. This can help healthcare organizations to understand the needs of their patients and make changes to promote healthcare access. Partner with community agencies, schools, or nonprofits to make screenings easier to attend.
- Encourage healthcare agencies to continually assess patient satisfaction through exit surveys or follow-up emails to improve the quality of treatment. Health Councils can promote continuous evaluation so that agencies can know and respond to make the healthcare experience suitable for all.
- Partner with your local non-profit hospital to connect the goals of the Community Health Assessment (CHA) with the hospital’s Community Health Needs Assessment (CHNA). The Affordable Care Act mandates that not-for-profit hospitals participate in CHNAs and develop strategies for community-identified needs every three years. Strengthening this relationship between the community and the hospital, can streamline resources and efforts within a community.
- Seek funding to improve access to telehealth services or improved digital technology to support telehealth. Telehealth can improve access to affordable health care, especially in rural areas where provider shortages interfere with care.
- Encourage healthcare institutions to actively participate in advocacy and systems change to promote health. Support agencies to prioritize initiatives that improve community conditions for healthier living. For example, health clinics can work to support road improvements for walking and cycling, increasing physical activity while creating another means of transportation for health visits.
- Support policy initiatives that address root causes of desired health goals. Conduct a root cause analysis to explore the factors that contribute to a particular health challenge for communities. Analyzing root causes can help communities to identify and tackle the underlying causes of health issues.
Sullivan County Regional Health Department - Trauma-Informed Workforce
In early 2022, the director of the Sullivan County Regional Health Department decided to take bold steps to embed a person-centered and trauma-informed lens into the day-to-day operations of their health department. Sullivan County, like many areas in the U.S., had been hit hard by the substance misuse and opioid epidemics, which has led to disruptions in the overall health of the county residents. Director Gary Mayes wanted to bring a trauma-informed lens to the department to improve care for patients and enhance the working environment for employees. Through a partnership with trauma-informed care consultant Becky Haas, the Health Department started a process to become a trauma-informed workforce. The Sullivan County Regional Health Department formed an implementation team of directors, nursing supervisors, and other staff members who took the lead on the following actions:
- Staff participated in trainings on trauma-informed care, workplace wellness, and best practices to understand the importance of trauma-informed care and bring it to life. A train-the-trainers model was used so staff can conduct trainings for other interested parties across the county.
- The implementation team conducted environmental scans of their facilities, finding ways to improve the space to be more inviting and help patients feel psychologically safe during their visits.
- Workforce wellness was encouraged by promoting daily walking during the workday, small changes to workstations such as calm lighting, and engaging in peer support groups.
- A new onboarding protocol was implemented, where new hires are brought into the trauma-informed mindset by engaging in training on ACEs and trauma during orientations and completing staff wellness surveys periodically during their first 3 months.
- Trauma-informed care was embedded into all job descriptions.
- Engaging in community outreach at women's health service centers, the local jail, and recovery clinics to expand the reach of the trauma-informed approach within public health was emphasized.
- A three-year workplan was produced to maintain commitment to sustainable trauma-informed practices.
Almost a year since the project started, the Sullivan County Regional Health Department has noticed the changes in culture and treatment due to their commitment to a trauma-informed workforce.
For more information, reach out to Becky Haas at becky@beckyhaas.com.
Trousdale County Mental Health Services Center
For the past few years, the Trousdale County Health Council has been collaborating with the Mayor's office to coordinate the Mayor's Task Force for Mental Health and Substance Abuse. In 2021, Trousdale County experienced 6 suicides - an alarming rate for a small community of 11,000 people. In response, the task force was formed to create a coordinated effort to bring mental health resources to the county. The task force is a multisector group with community involvement from faith-based organizations, behavioral health organizations such as Centerstone and Volunteer Behavioral Health, the sheriff and district attorney, and more. At the time the task force was being formed, there were virtually no mental health resources available in the entire county.
One of the key goals of the task force was to procure a building to offer mental health services where providers could have a home base. Through the partnership with the mayor's office and the county, the task force received funding for $80,000. The task force found a space where services could be offered in a building that also houses a pharmacy and a medical provider, helping to eliminate small town stigma from keeping people from services. They partnered with multiple behavioral health providers to share the space so that individuals could seek treatment from any of the available providers - including Volunteer Behavioral Health, Centerstone, HOPE Clinic, and Senior Solutions. The new mental health services center celebrated their kickoff in June 2023, and have already enrolled various community members to receive services. The original funding will support the project for the initial pilot period of 2 years, with the hope that the mental health services center can become embedded into the Trousdale community for years to come. This successful collaboration between the Health Council, the Mayor's office, and multiple community partners is already making a difference in access to mental health providers in Trousdale county.
For more information, contact Kathy Atwood at kathyatwood@tcschools.org
TN Department of Health
- Local Health Departments across the state operate to address community health needs in all 95 counties of Tennessee. Local health departments are ideal partners for health councils to collaborate to improve health in local communities
- Family Health and Wellness
- Women, Infants, and Children Program (WIC) provides access to nutrition assistance, nutrition education, breastfeeding education and support, and healthcare referrals for mothers of young children, helping to meet basic health needs during the transition to having a child.
- Community Health Access and Navigation in Tennessee (CHANT) provides care coordination through local health departments. Eligible individuals are connected to resources and support for their health and medical needs, such as reimbursement or assistance with co-pays. CHANT can help individuals to access medical care to improve their health who may otherwise not be able to afford it.
- Division of Health Disparities Elimination - Tennessee Healthy Smiles Initiative:
- Smile on 65+: Through a partnership with the interfaith Dental Clinic, the Smile on 65+ program provides statewide oral health care and case management services for older adults.
- Tennessee Dental Safety Net Denture Program: State funds support some of the costs of dentures for working age Tennesseans (18-64) seen in charitable care clinics.
- Tennessee State Loan Repayment Program (TSLRP): TSLRP provides educational loan repayment to primary care physicians, Dentists, Advanced Practice nurses, Physican Assistants, Primary Care Behavioral Health and Mental Health Professionals, and Pharmacists (Pharm-D) who qualify in exchange for a 2-year service obligation to practice either full-time or part-time at an ambulatory non-profit, public or private non-profit primary care site that is located in a federally designated Health Professional Shortage Area (HPSA), rural health clinic (RHC), or Federal Qualified Health Center (RQHC).
TN Division of TennCare
- TennCare is Tennessee's Medicaid program that provides health insurance to those who are eligible for Medicaid. TennCare provides health insurance for roughly 1.7 million Tennesseans which covers about 23% of the population, 50% of the state's births and 53% of children in the state. As of January 1, 2023 all adults on TennCare now have dental benefits. More info here (link).
- CoverKids is Tennessee’s CHIP program which provides health insurance for children aged 18 and younger or pregnant women who fit eligibility requirements.
- The Presumptive Eligibility program provides temporary TennCare coverage to people who meet certain medical and eligibility criteria including pregnant people and those diagnosed with breast of cervical cancer.
TN Department of Mental Health and Substance Abuse Services
- Project Rural Recovery: TDMHSAS and community behavioral health providers Buffalo Valley Inc (Middle Tennessee) and McNabb Center (East Tennessee) are addressing behavioral and physical health needs for those living in 10 specified rural counties through Tennesseans Project Rural Recovery. Providers participating in this program built and then will operate mobile health clinics that will travel to the counties they serve, set up clinics, and hold appointments. Project Rural Recovery offers a variety of services including physical health services, mental health services, and substance use services.
- Behavior Health Safety Net (BHSN): Individuals 3 years of age or older who have a qualifying mental health diagnosis and have no behavioral health insurance may qualify for the Behavioral Health Safety Net (BHSN) of TN program. Services that are provided by this program include assessment, evaluation, diagnostic, therapeutic intervention, case management, transportation, peer support services, psychosocial rehabilitation services, psychiatric medication management, labs related to medication management, and pharmacy assistance and coordination.
U.S. Department of Housing and Urban Development
- Free Or Low-Income HealthCare in Tennessee is a statewide list of healthcare centers and service providers that offer care for uninsured, underinsured, or homeless individuals.
Tennessee Alliance of Oral Health Advocates
- Safety Net Dental Clinic Directory provides a list of dental clinics based on varying levels of patient insurance acceptance.
National Institute for Healthcare Management
- Rural Health: Addressing Barriers to Care provides insightful infographics on the state of healthcare access in rural America.
The Picker Institute
- The Picker Principles of Person Centred Care describe the eight elements of PCC in depth, with additional resources and research.
Center for Health Care Strategies
- Trauma-Informed Care Implementation Resource Center includes resources on multiple topics under the umbrella of TIC, including how to invest in a trauma-informed workforce.
Department of Health and Human Services
- Think Cultural Health provides tools and trainings on culturally and ligustically appropriate services, health equity communications, and policies regarding cultural competency.
SAMSHA
- Key Ingredients for Successful Trauma-Informed Care Implementation outlines important elements to implementing TIC approaches in organizations and clinical practices.