Healthy Places - Health Disparities
Health disparities are differences in quality of health and availability of health care between populations. Health disparities come from a variety of factors such as individual behaviors, genetics and environmental risks. These differences are often related to social, economic and environmental disadvantages. Differences in health and health care between groups of people can be social justice and health equity issues. Many health disparities are considered avoidable. Communities that understand and respond to health disparities benefit both individual and population health. Improving health disparities reduces unnecessary health care costs.

Define health disparities?
What populations are effected by health disparities?
What are social determinants of health?
Why illnesses show disparities?
What about asthma disparities?
What contributes to environmental disparities?
What tools are available?
What can schools do about disparities?
Are there health disparities in my community?
Government partners
Additional resources
Define health disparities?
The Kaiser Family Foundation provides helpful definitions. Health and health care disparities refer to differences in health and health care between population groups.
health disparity – higher burden of illness, injury, disability or mortality experienced by one population group relative to another group
health care disparity – differences between groups in health coverage, access to care and quality of care
While disparities are commonly viewed through the lens of race and ethnicity, they occur across many dimensions, including socioeconomic status, age, location, gender, disability status and sexual orientation.
What populations are affected by health disparities?
Health disparities affect many people. Some populations to whom health or health care disparities have been witnessed include Native Americans, black and African American, Hispanic and Latino, the disabled, low-income, less educated, and people who live in rural areas.
What are social determinants of health?
According to the CDC, the conditions in the places where people live, learn, work and play affect a wide range of health risks and outcomes. These conditions are known as social determinants of health. For example, poverty is a social determinant of health. Poverty limits access to healthy foods and safe neighborhoods. Educational attainment is one of the most important predictors of better health. Understanding social limitations can improve health equity. Responding to social determinants of health can improve individual and population health.
The CDC’s Social Determinants of Health website provides resources for data, tools for action, programs and policy. It can be helpful for people in public health, community organizations and health care systems to assess social determinants of health and improve community well-being.
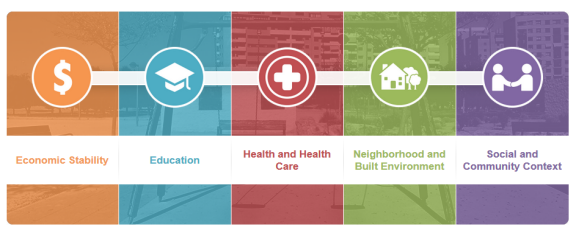
Healthy People 2020 has the goal to create social and physical environments that promote good health for all. Healthy People 2020 organizes the social determinants of health around five key domains: (1) economic stability, (2) education, (3) health and healthcare, (4) neighborhood and built environment, and (5) social and community context.
What illnesses show disparities?
Some illnesses have been shown to be more common in certain groups of people. Some of the higher burden of illness, injury, disability or mortality has been measured in asthma, cancer, diabetes, infant mortality and heart disease.
What about asthma disparities?
Asthma affects many households. Some people experience asthma more severely than others. Significant differences in asthma exist for some racial and ethnic groups. For example, due to asthma attacks black children are hospitalized at twice the rate of white children. Children from low-income or minority families are at greater risk to have the disease and for more severe symptoms. The Department of Health’s Asthma Management Initiative works to promote lung health and reduce asthma disease and disparities. The Environmental Protection Agency’s asthma webpage promotes understanding and management of asthma. Both webpages have resources and toolkits available children, parents, providers, schools and communities. Places can be designed and maintained to reduce environmental asthma triggers such as secondhand smoke to help reduce the burden of asthma.
What contributes to environmental disparities?
Some communities have a higher burden of environmental hazards such as air pollution or hazardous waste sites. Here are some factors that may contribute to environmental disparities:
- cumulative or multiple exposures to environmental hazards,
- low social and economic status,
- limited access to community resources,
- land-use patterns,
- quality of and access to health care,
- substandard housing,
- crowding,
- community stress,
- residential segregation, or
- lack of resources such as grocery stores with healthy foods.
What tools are available?
Health disparities affect quality of life in vulnerable communities. CDC and TDH promote best public health practices to safeguard all people. Health Impact Assessments (HIAs) are a tool to bring potential public health concerns to the decision-making process for plans, projects and policies that fall outside the traditional public health arenas, such as local transportation and land use. HIAs help vulnerable communities reduce health costs by recommending proven public health approaches that meet their needs while offering training and technical assistance.
What can schools do about disparities?
Health disparities are related to inequities in education. Since educational attainment is connected to health, schools can be a place to reduce disparities. According to the CDC’s Division of Adolescent and School Health, schools help to evenly distribute social, political, economic and environmental resources. For example, dropping out of school is associated with social and health problems. Individuals with higher educational attainment often have less health risks from smoking, substance abuse, obesity and injury. Schools can be a place for children and adolescents to start learning how to understand and access health information and services needed throughout life to make health and health care decisions.
Are there health disparities in my community?
Communities with unstable housing, low income, unsafe neighborhoods or substandard education are more likely have health disparities. Understanding what health disparities may exist can help your community locate data. One place to look for data is the Tennessee Department of Health’s 2015 Drive Your County to the Top Ten special reports. Each report shows the rank each county holds compared to other counties on a number of health outcomes. The Healthy People 2020 Objective Data webpage lists several social determinants of health. Refer to the Healthy Places Data and Indicators webpage for more ideas.
Government partners
Tennessee Department of Health (TDH)
Division of Minority Health and Disparities Elimination
www.tn.gov/health/health-program-areas/dmhde.html
Centers for Disease Control and Prevention (CDC)
Health Disparities & Inequalities Report (CHDIR)
www.cdc.gov/minorityhealth/chdireport.html
Office of Minority Health
www.cdc.gov/minorityhealth
Social Determinants of Health: Know What Affects Health
www.cdc.gov/socialdeterminants/index.htm
ChangeLab Solutions
Webinar: Health Equity
www.changelabsolutions.org/publications/the-series_episode-1
Additional resources
The Kaiser Family Foundation
Disparities Policy
kff.org/disparities-policy/issue-brief/disparities-in-health-and-health-care-five-key-questions-and-answers